Histamine Intolerance: What’s the gut got to do with itchy skin?
Trying to understand the complexity of how your gut could be causing your itchy skin takes you into the wonderful world of the workings of your gastrointestinal tract (gut) and the microorganisms that live there. These microorganisms make up your microbiome. This century, science has done a great job of uncovering this world of microbes within, and all the important things they do for your health. These healthy gut flora are important in maintaining the function of your gut lining which is critical for keeping pathogens out and helping you absorb nutrients. Your microbiome also acts as the overseers of your immunity; they’re important in making neurotransmitters to keep you balanced and chill; and they even make some vitamins for you. Getting back to itchy skin, it’s important to keep a healthy well-balanced microbiome. Your microbiome needs looking after, so that it stays in healthy balance and can work well for you. Many influences can disrupt this balance and cause an overgrowth of bacterial microbes in your gut, called dysbiosis. Among other things, a dysbiosis will ferment proteins, and produce histamine. This production of histamine is in excess of what your own cells produce as part of a healthy immune response.Histamine is an important part of your immune response in appropriately small amounts. Histamine opens the blood vessel pathways so your army of white blood cells can eliminate pathogenic infiltrators. In a healthy balanced body, histamine production stays relatively low and any slight over-production of histamines will be cleared by two naturally produced enzymes, Diamine Oxidase (DAO) and Histamine-N-methyl Transferase (HNMT). However, high levels of histamines produced by dysbiotic bacteria, can over-face these enzymes and cause all sorts of allergy responses including itching. Itching is the trademark of the high histamine levels found in histamine intolerance (HIT). Other HIT symptoms include diarrhoea/constipation, IBS, gut pain, nausea and vomiting and heat/flushing. Tummy aches; carsickness and ‘one red ear’ in children are strong indicators of HIT.Most foods contain some histamine, and even helpful bacteria may produce a little histamine, so it’s important to consider many things when faced with histamine intolerance. Factors that contribute to HIT…
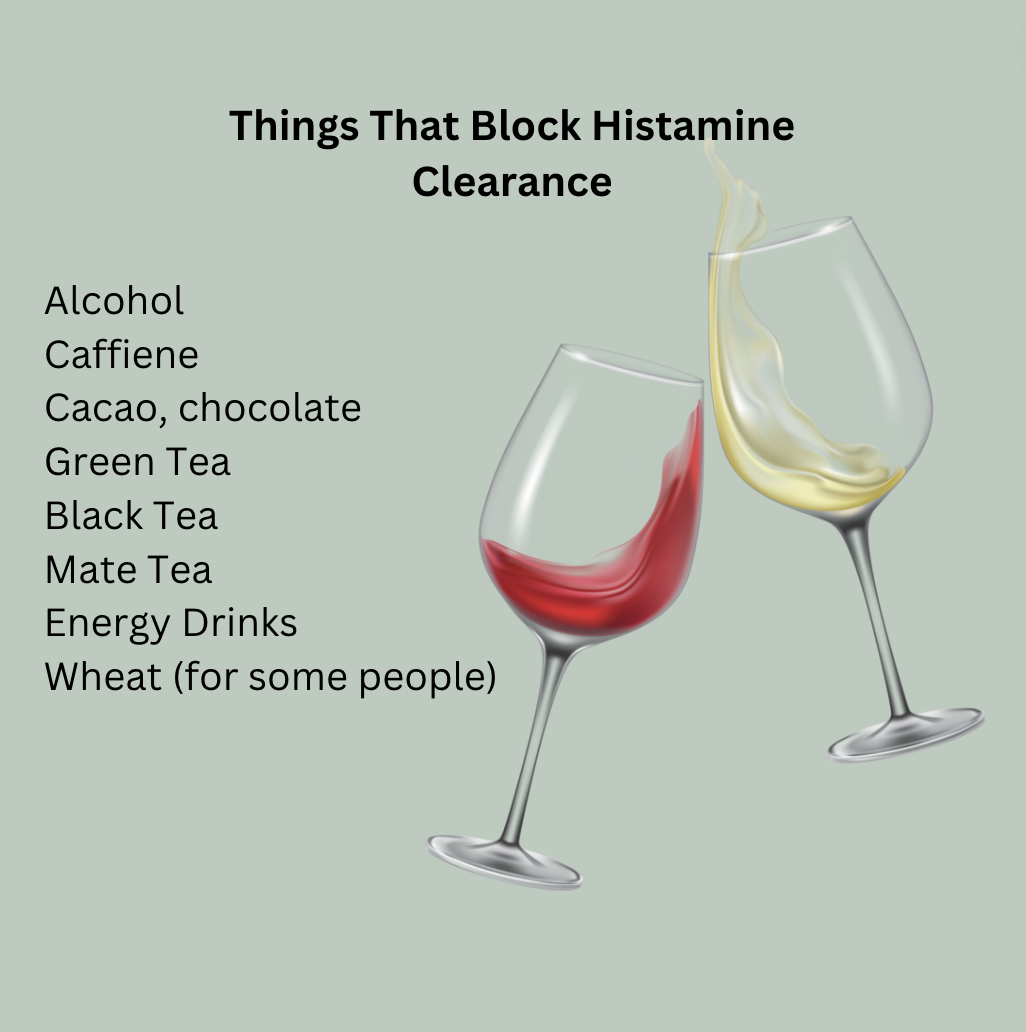
Anything that increases natural histamine production to excess – inflammation, stress and injury will do this, some foods also stimulate histamine release.Anything that inhibits the work of DAO and HNMT (the naturally produced enzymes that break down histamine) – this includes genetic variations, some medications (eg Ibuprofen, voltaren), alcohol, and some foods.Excessive high histamine foods – but if someone has become extremely intolerant, some low histamine foods may also cause symptoms.Dysbiotic gut bacteria which produce histamines that are absorbed into the bloodstream through a ‘leaky’ gut barrier – here too it get’s tricky as even helpful microbes may produce histamine (think twice about kombucha if you show histamine symptoms!).Changing hormonal states – oestrogen can cause something called mast cell degranulation, which increases histamine release, and histamine can increase oestrogen production! That’s definitely a vicious cycle that needs to be regulated!
The good news is that histamine intolerance can be reversed. With a concerted effort you can heal and bring your body into healthy balance. This may only take a few weeks, with some ongoing regulation for maintaining healthy balance.So, what to do?
Minimise inflammation and stress, and where possible treat injuries with effective natural processes not histamine producing medications.
Minimise foods that stimulate histamine release (see below).
Avoid using Ibuprofen, voltaren and other DAO inhibitors, these foods block DAO and keep histamine in your system (see below)
Support the production of your HNMT enzyme by supporting methylation.
Avoid excessive high histamine foods (see below).
Learn how to support a healthy microbiome – what to feed them and how to protect them.
Take targeted gut healing products to ensure your gut barrier is functioning well.
Support healthy hormonal balance – get professional help if needed.
Some people with histamine intolerance cannot tolerate dairy at all. Others tolerate small amounts